0
The serotonin theory of depression: a systematic umbrella review of the evidence - Molecular Psychiatry
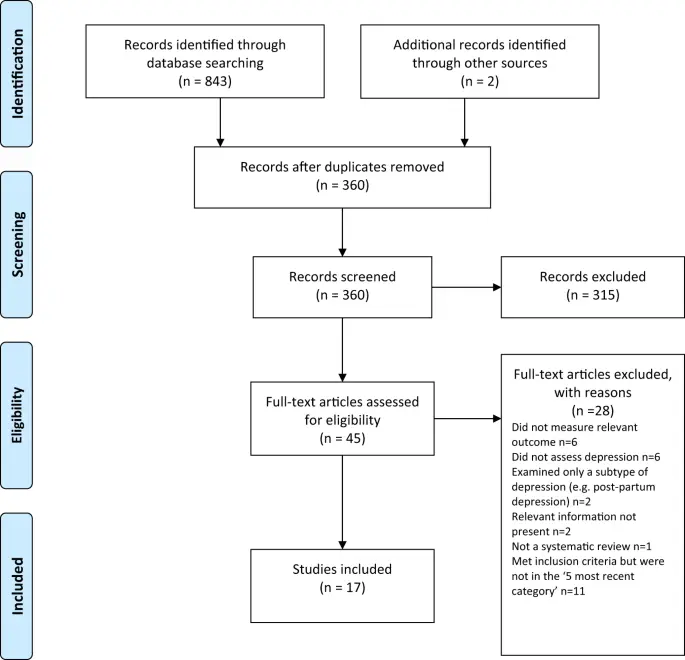
www.nature.comThe serotonin hypothesis of depression is still influential. We aimed to synthesise and evaluate evidence on whether depression is associated with lowered serotonin concentration or activity in a systematic umbrella review of the principal relevant areas of research. PubMed, EMBASE and PsycINFO were searched using terms appropriate to each area of research, from their inception until December 2020. Systematic reviews, meta-analyses and large data-set analyses in the following areas were identified: serotonin and serotonin metabolite, 5-HIAA, concentrations in body fluids; serotonin 5-HT1A receptor binding; serotonin transporter (SERT) levels measured by imaging or at post-mortem; tryptophan depletion studies; SERT gene associations and SERT gene-environment interactions. Studies of depression associated with physical conditions and specific subtypes of depression (e.g. bipolar depression) were excluded. Two independent reviewers extracted the data and assessed the quality of included studies using the AMSTAR-2, an adapted AMSTAR-2, or the STREGA for a large genetic study. The certainty of study results was assessed using a modified version of the GRADE. We did not synthesise results of individual meta-analyses because they included overlapping studies. The review was registered with PROSPERO (CRD42020207203). 17 studies were included: 12 systematic reviews and meta-analyses, 1 collaborative meta-analysis, 1 meta-analysis of large cohort studies, 1 systematic review and narrative synthesis, 1 genetic association study and 1 umbrella review. Quality of reviews was variable with some genetic studies of high quality. Two meta-analyses of overlapping studies examining the serotonin metabolite, 5-HIAA, showed no association with depression (largest n = 1002). One meta-analysis of cohort studies of plasma serotonin showed no relationship with depression, and evidence that lowered serotonin concentration was associated with antidepressant use (n = 1869). Two meta-analyses of overlapping studies examining the 5-HT1A receptor (largest n = 561), and three meta-analyses of overlapping studies examining SERT binding (largest n = 1845) showed weak and inconsistent evidence of reduced binding in some areas, which would be consistent with increased synaptic availability of serotonin in people with depression, if this was the original, causal abnormaly. However, effects of prior antidepressant use were not reliably excluded. One meta-analysis of tryptophan depletion studies found no effect in most healthy volunteers (n = 566), but weak evidence of an effect in those with a family history of depression (n = 75). Another systematic review (n = 342) and a sample of ten subsequent studies (n = 407) found no effect in volunteers. No systematic review of tryptophan depletion studies has been performed since 2007. The two largest and highest quality studies of the SERT gene, one genetic association study (n = 115,257) and one collaborative meta-analysis (n = 43,165), revealed no evidence of an association with depression, or of an interaction between genotype, stress and depression. The main areas of serotonin research provide no consistent evidence of there being an association between serotonin and depression, and no support for the hypothesis that depression is caused by lowered serotonin activity or concentrations. Some evidence was consistent with the possibility that long-term antidepressant use reduces serotonin concentration.


I had it bad, like almost 0 functioning ability, and nothing worked before ketamine. So personally checks out.
I read one reason ssris could still work for some people is because for one they are actually pretty good at reducing anxiety symptoms, but also just because serotonin deficiency isn’t the cause of depression doesn’t mean that increasing serotonin can’t improve your mood at all.
Hey! Would be curious about your experience with ketamine. My partner is looking to get treatment. Personally I’ve done tons of mushrooms , a little LSD, but never ketamine. Shes used mushrooms once and it was really difficult but ultimately healing (her words). She’s resistant to trying SSRIs entirely (i support this 100%) and is looking for alternatives to approaches that medicalize/pathologize trauma.
To start I have to say it can be pretty expensive. I’m in the US and insurance won’t cover it, they can’t get IV ketamine “approved” for depression because there’s no money to be made off the drug itself because of how old it is. It’s one of the cheapest drugs to make so the money is just for the people watching you sit there I guess. There’s nasal spray “esketamine” which my doctors don’t recommend bc with IV its easier to control the dose, that got approved because it has a patent, so it’s technically possible to get that covered but in my experience providers of that also choose to not take insurance.
I’m sure you could find a doctor with any kind of opinion but mostly they don’t use it as a first line of treatment because of how involved it is. So I’m not sure if someone who hasn’t been on any antidepressants before would have good chances getting it prescribed. A couple years ago I read a lot of things where they were recommending it to treatment resistant patients mostly, which is 3+ meds unsuccessful. Also most doctors will want you to be on another antidepressant aside from the ketamine. I stopped taking mine without mentioning it because it wasn’t doing anything. lol
As for the actual treatment. It takes like an hour and they give you a little bit every 10 minutes or so and then just let you sit until you’re good to leave. It’s an anesthetic so she should have someone go with her because she’ll probably be disoriented for a little bit. The half life is very short though so any side effects should be gone within a couple hours. I’ve seen people online talk about it like being high or about “k holes” or w/e but I think they’re being dramatic. When I get it I feel a little out of it, kinda physically numb, and the room does look a bit strange as if the distance between everything and/or size of objects has been altered slightly, but nothing too serious. You mentioned she has trauma. If she has any significant amount of dissociative symptoms from that then her brain probably hits her with way more heavy experiences than the small amount of ketamine would, at least that’s how it is for me. I usually text or read things online the whole time idk.
Symptom relief is pretty immediate. Your mood improves within a few hours usually. For people currently in an episode getting treatment for the first time they get a bunch of treatments every few days for a couple weeks. It’s not always long lasting, some studies say there’s a drop off after like 2 weeks no treatment. But most doctors that do it say people can usually start spreading out appointments much longer than that. I get a headache afterwards until I sleep it off so usually I notice the difference in symptoms from when I wake up from that. lol Since I started it I can kinda enjoy things again whereas before treatment I had stopped bothering to even try playing video games anymore, and those things are designed to keep your constant attention with little dopamine hits. I can hold a job now, even if it’s not always easy (I do have other physical and mental health issues so I can’t say how much is lingering depression). I even can focus enough to read sometimes. No suicide attempts since, almost no self harm and if it was it from ptsd so it had a clear trigger. I remember to eat more often and take care of hygiene. I socialize more. Pretty much everything is much better, not perfect of course but yeah.
I think that about covers what I can say without being prompted by more specific questions. lol